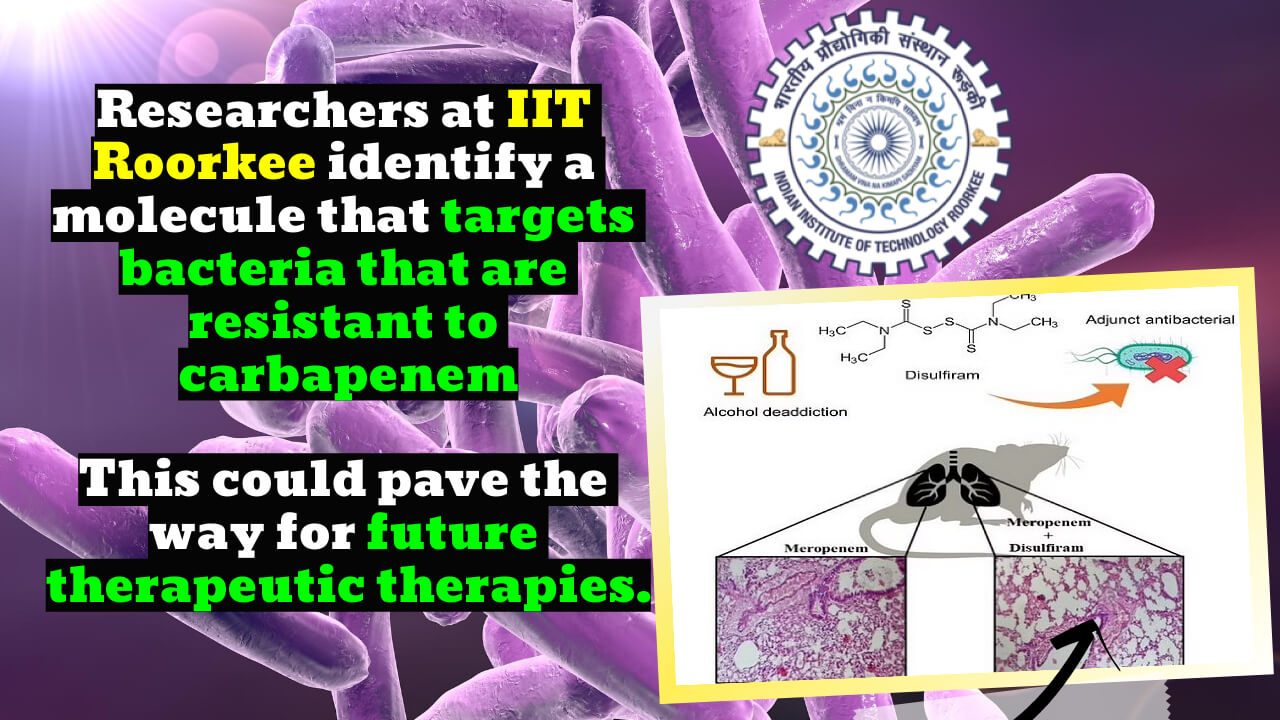
Disulfiram inhibits Metallo-b-lactamase, an enzyme that neutralizes last-resort carbapenems. The study was published in the Journal of Antimicrobial Chemotherapy. Disulfiram can boost the efficacy of Meropenem, a popular antibiotic for bacterial infections. Carbapenem-resistant Acinetobacter baumannii with NDM and IMP.
Key Highlight:
- The Indian Institute of Technology, Roorkee (IIT Roorkee) has discovered a novel method of Disulfiram in treating blood infections and pneumonia caused by the nosocomial bacterium Acinetobacter baumannii.
- According to PRO, a team led by Prof. Ranjana Pathania of IIT Roorkee revealed that Disulfiram can inhibit Metallo-b-lactamase, an enzyme that neutralizes last resort carbapenem antibiotics.
- Carbapenem-resistant Acinetobacter baumannii is more resistant to disulfiram than other antibiotics.
- The researchers employed multiple methods to assess the bacteria’s antibiotic susceptibility and found that Disulfiram can make Meropenem, a routinely used antibiotic, more effective against Carbapenem-resistant Acinetobacter baumannii.
- Combined disulfiram-carbapenem trials may pave the way for future treatments.
Disulfiram’s unique mode of treating blood infections and pneumonia caused by the metallo-beta-lactamase producing Acinetobacter baumannii, a nosocomialtop priority pathogen, has been deciphered by researchers at the Indian Institute of Technology, Roorkee (IIT Roorkee).
It turns out that the drug Disulfiram can stop an enzyme called Metallo-b-lactamase from working properly. This enzyme neutralizes the last-ditch carbapenem antibiotics. The research team led by Prof. Ranjana Pathania found this out.
Disulfiram, on the other hand, makes the Carbapenem class of antibiotics more effective against Acinetobacter baumannii, which is resistant to carbapenem.
The study by Vineet Dubey, Kuldip Devnath, Mangal Singh, Prof. Ranjana Pathania, and other people working in the Molecular Bacteriology and Chemical Genetics lab at IIT Roorkee has been published by Oxford University Press in the Journal of Antimicrobial Chemotherapy, which is a journal.
Acinetobacter baumannii is a big problem in hospitals worldwide, and it’s not just in the United States. This is because it is one of the main causes of infections in people who use hospital ventilators and invasive devices, like urinary catheters, to get better.
63% of infections are caused by the multidrug-resistant strains of this bacterium, which is the main concern because it has become more resistant to antibiotics.
For this reason, the World Health Organization (WHO) has made research and development of new drugs for this pathogen a top priority this year.
Disulfiram, a common antibiotic used to treat bacterial infections, can make Meropenem more effective against bacteria that make New Delhi Metallo-b-lactamase (NDM) and Integral Membrane Protein (IMP) that are resistant to Carbapenem. The study said that research on disulfiram and carbapenem together could lead to new clinical treatments.
Antibiotic-resistant microbial infections are a big problem for people all over the world. The director of IIT Roorkee, Prof. Ajit K Chaturvedi, said, “This research is a glimmer of hope because it has opened up new ways to treat infections of the blood and other body parts caused by these pathogens.”
Disulfiram is a drug that the FDA has approved. It is used to help people who have been drinking for a long time stop drinking.
When the team looked at Carbapenem monotherapy and Carbapenem therapy in combination with Disulfiram, they found that the combination group had better results in getting rid of bacteria in mice’s bodies.
They worked together against NDM, and IMP-producing Carbapenem-resistant Acinetobacter baumannii (CRAb) isolates in time-kill analysis, which looks at how many bacteria there are in a certain environment.
The combination was better at getting rid of bacteria from the liver and spleen of mice infected with IMP-expressing CRAb than either one alone. “The combination significantly cut down on the number of bacteria that were NDM producers in the pneumonia model, compared to just giving them antibiotics.”